When it comes to strokes, recognizing symptoms quickly can make all the difference between recovery and permanent disability. This comprehensive guide will help you identify stroke signs and take appropriate action during those critical first moments.
What happens during a stroke?
Your brain needs a constant supply of oxygen-rich blood to function properly. During a stroke, this flow gets interrupted in one of two ways:
- Blood vessels become blocked (ischemic stroke)
- Blood vessels rupture and bleed (hemorrhagic stroke)
Without oxygen, brain cells begin dying within minutes, which is why immediate recognition and response are vital.
The FAST method explained
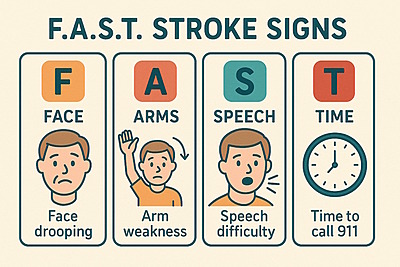
Medical experts developed the FAST method as a simple memory tool to help everyday people recognize the most common stroke symptoms. Here’s what each letter stands for:
F: Face Changes
Look for unexpected changes in facial appearance. Request that the individual grin or display their teeth. During a stroke, muscles on one side of the face may not work properly.
Watch for:
- One corner of the mouth drooping lower than the other
- An uneven smile that looks lopsided
- One eyelid that appears to sag
- Numbness that makes one side of the face appear frozen
A: Arm Movement
Arm weakness or numbness often affects just one side of the body during a stroke. This one-sided pattern is a key indicator.
Test by asking the person to:
- Raise both arms straight out in front of them
- Close their eyes while holding this position for 10 seconds
Watch for:
- One arm drifting downward while the other stays up
- Inability to lift one arm completely
- Complaints of heaviness or numbness in one arm
- Difficulty gripping objects with one hand
S: Speech Problems
Stroke often affects language centers in the brain, causing noticeable speech changes that weren’t present before.
Listen for:
- Words that sound thick or slurred
- Sentences that don’t make logical sense
- Using incorrect or made-up words
- Difficulty understanding simple instructions
- Complete inability to speak despite being awake
Ask the person to repeat a simple sentence like “The sky is blue today.” Pay attention to how clearly they pronounce the words and whether the sentence makes sense.
T: Time for Emergency Action
If you notice any of these warning signs, don’t wait to see if they improve. Call emergency services immediately.
Important time-related points:
- Note exactly when symptoms began (check the time)
- Stroke treatments work best within the first few hours
- Even if symptoms seem to improve, still seek emergency care
- Never drive yourself or the affected person to the hospital
Beyond FAST: additional warning signs
While FAST covers the most common and recognizable symptoms, be aware of these other possible stroke indicators:
Sudden Balance Problems
- Unexpected dizziness or vertigo
- Stumbling without an obvious cause
- Difficulty walking in a straight line
- Leaning heavily to one side when standing
- Falling without tripping on anything
Vision Disturbances
- A reduction or total loss of sight in one or both eyes
- Double vision that appears suddenly
- Inability to see things on one side (like seeing only half of a person’s face)
- Blurred vision that wasn’t present before
Unusual Headache
- Intense pain that strikes without warning
- Headache unlike any experienced before
- Pain described as “explosive” or “thunderclap”
- Headache accompanied by nausea or vomiting
Mental Confusion
- Sudden disorientation about time, place, or situation
- Inability to recognize familiar people
- Trouble understanding conversations
- Inappropriate emotional responses
- Personality changes that seem out of character
Emergency response steps
If you suspect someone is experiencing a stroke, follow these steps:
- Call emergency services immediately. Don’t call family members first or wait to see if symptoms improve.
- Document the timeline. Make note of exactly when symptoms first appeared. This information directly impacts treatment options at the hospital.
- Position the person safely
- Help them lie down with head and shoulders slightly elevated
- Turn them onto their side if they’re vomiting
- Loosen tight clothing around the neck
- Monitor breathing and consciousness
- If the person becomes unconscious but is breathing, place them in recovery position (on their side)
- If breathing stops, begin CPR if you’re trained
- Be prepared to provide this information when help arrives
- What NOT to do:
- Don’t give food or drinks (even water)
- Don’t administer any medications
- Don’t let the person go back to sleep “to feel better”
- Don’t delay calling for help, even if symptoms seem mild
Special situations: when you’re alone
If you live by yourself or spend significant time alone:
Preparation steps:
- Program emergency contacts into your phone with one-touch dialing
- Consider wearing a medical alert device with fall detection
- Share your schedule with neighbors or family members
- Always ensure your phone is charged and easily accessible
If you experience symptoms while alone:
- Call emergency services immediately, before symptoms potentially worsen
- Unlock your door if possible so responders can enter
- Move to the floor in a safe position if you feel unsteady
- If you can’t reach a phone, use any emergency alert system or make loud noises to attract attention
Caring for someone at high risk
If you live with or care for someone with stroke risk factors:
- Learn how to take their blood pressure
- Help them maintain medication schedules
- Know their normal behavior patterns so changes are obvious
- Post emergency numbers in visible locations
- Create a health information card listing their conditions and medications
- Practice what you would do in an emergency
Different types of stroke
Ischemic stroke
These occur when blood clots or other particles block vessels supplying blood to the brain. They represent the majority of stroke cases and respond well to early treatment with clot-dissolving medications.
Hemorrhagic stroke
These happen when a weakened blood vessel ruptures, causing bleeding into or around the brain tissue. Though less common, they’re often more dangerous and require different treatment approaches than ischemic strokes.
Transient ischemic attack (TIA)
Sometimes called a “warning stroke,” TIAs produce stroke-like symptoms that resolve within minutes to hours. Even though symptoms disappear, immediate medical attention is crucial as TIAs often signal an impending full stroke.
Risk factors worth knowing
Understanding these risk factors can help you take preventative actions:
Things you can change
- Untreated high blood pressure
- Smoking and tobacco use
- Poorly controlled diabetes
- Physical inactivity
- Excessive alcohol consumption
- Poor diet high in sodium and unhealthy fats
- Untreated sleep apnea
- Stress management issues
What you cannot change
- Age (risk increases with age)
- Family history of stroke
- Previous stroke or TIA
- Gender (risk varies by age and stroke type)
- Certain genetic conditions
Common questions and answers
Q: Can someone appear normal between stroke symptoms?
A: Yes. Some people experience intermittent symptoms that come and go before a major stroke. Any temporary stroke-like symptom requires immediate medical evaluation.
Q: Do strokes always affect one side of the body?
A: While one-sided symptoms are common and distinctive signs of stroke, some strokes can cause symptoms affecting both sides or other patterns depending on which brain areas are involved.
Q: Is stroke always painful?
A: Most strokes are not painful, which sometimes delays people seeking help. Only certain types (particularly hemorrhagic strokes) might cause severe headache.
Q: Can children have strokes?
A: Yes, though much less commonly than adults. Children’s stroke symptoms may include seizures, sudden weakness, severe headaches, or unexplained dizziness.
Remember: When it comes to stroke response, it’s always better to err on the side of caution. Emergency medical providers would rather evaluate someone who turns out to be fine than miss the opportunity to provide life-saving treatment during the critical window.
