The F22 diagnosis in the ICD-10 stands for “Delusional Disorder”. This psychiatric condition is characterized by the presence of persistent, non-bizarre delusions lasting at least one month or longer. These delusions are typically not accompanied by significant mood disorders, hallucinations, or other symptoms of psychosis that would suggest schizophrenia.
Delusional disorder is a rare psychiatric condition where the patient experiences persistent delusions without other prominent symptoms of psychosis like hallucinations, disorganized thought, or mood disturbances. It primarily affects adults, with the exact cause being multifactorial, including genetic predisposition, environmental stressors, and neurobiological factors.
Key symptoms
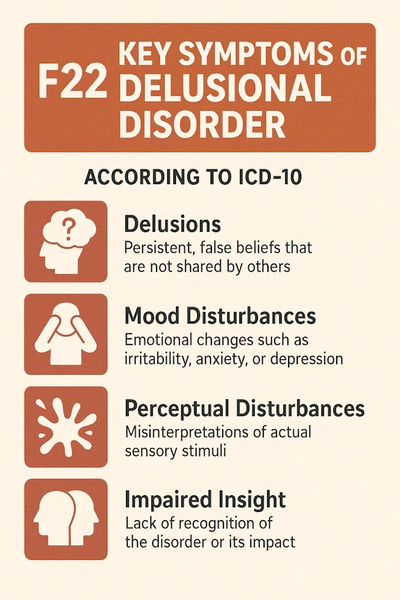
Delusions
The central feature is one or more delusions, which are fixed false beliefs not in keeping with reality or cultural norms.
-
- Examples include beliefs of persecution, grandiosity, jealousy, somatic concerns (e.g., believing one has a serious illness), or erotomania (believing someone is in love with them).
- Central to the diagnosis.
- They usually involve things that could really happen in real life, like being followed, getting sick from something bad to eat, or someone tricking you.
- Themes of delusions can vary widely but are often consistent within the individual’s belief system.
- Examples include beliefs of persecution, grandiosity, jealousy, somatic concerns (e.g., believing one has a serious illness), or erotomania (believing someone is in love with them).
Subtypes of delusions
- Persecutory: Belief of being harmed, conspired against, or targeted (e.g., “My neighbor is poisoning my food”).
- Grandiose: Belief in having exceptional abilities, wealth, or influence (e.g., “I am destined to be the world leader”).
- Erotomanic: Belief that someone, often of higher status, is in love with the individual (e.g., “This celebrity is secretly in love with me”).
- Jealous: Conviction that a partner is unfaithful despite a lack of evidence.
- Somatic: False belief about physical health or bodily functions (e.g., “I have worms under my skin”).
- Mixed or Unspecified: Delusions that do not fit neatly into one category or involve multiple themes.
Apart from the delusions, the person’s thoughts, emotions, and behaviors are often relatively normal. They may seem coherent and rational when discussing topics unrelated to the delusion.
- Hallucinations, if present, are usually limited and related to the delusional theme (e.g., hearing voices of a persecutor in a delusion of persecution).
- There are no prominent disorganized thoughts or behaviors.
Delusional disorder often has a chronic, long-term course, but the specific delusions may change over time.
The delusions are not better explained by another condition, such as schizophrenia, major depressive disorder with psychotic features, or a medical condition like dementia.
Detailed clinical features
- Preservation of other functions:
- The person’s speech, logical reasoning (outside the delusional theme), and behavior can appear normal.
- Social and occupational functioning may remain intact unless the delusions interfere.
- Minimal hallucinations:
- Hallucinations, if present, are usually brief and related to the delusional content (e.g., hearing threatening whispers in a persecutory delusion).
- Chronic and insidious onset:
- Symptoms often develop gradually and persist for months or years.
- It is often not recognized until the delusions start causing significant impairment or distress.
Diagnostic criteria (ICD-10 and DSM-5)
To diagnose Delusional Disorder, the following criteria must be met:
- Presence of one or more delusions lasting at least one month.
- These delusions are deeply held despite evidence to the contrary.
- Absence of schizophrenia:
- No prominent hallucinations, disorganized speech, or other symptoms that define schizophrenia.
- Minimal functional impairment:
- Outside of the delusional themes, the individual’s cognitive and social abilities are largely preserved.
- Not due to substances or medical conditions:
- Rule out delusions caused by drug use, brain injury, or other medical conditions.
- No significant mood disturbance:
- If mood symptoms (e.g., depression) are present, they are brief compared to the duration of the delusions.
Causes and risk factors
- Biological:
- Dysregulation in dopamine pathways in the brain.
- Structural abnormalities in brain regions (e.g., prefrontal cortex).
- Psychological:
- Low self-esteem and sensitivity to rejection.
- Personality traits like suspiciousness or rigidity.
- Environmental triggers:
- Stressful life events, trauma, or social isolation.
- The things people believe and how they act in their culture can change the way they think about things that aren’t real.
- Genetic influence:
- A family history of psychiatric disorders, especially schizophrenia, increases risk.
Course of the disorder
- Chronic Condition: Delusions can persist for years or even a lifetime without treatment.
- Periods of Remission: Some individuals experience partial or complete relief of symptoms intermittently.
- Impact on Life: Delusional disorder can lead to social isolation, strained relationships, and reduced quality of life.
Treatment
F22 is distinct from disorders like schizophrenia, as it lacks the severe disorganization, negative symptoms, and full-blown psychosis typical of that condition. If untreated, however, delusional disorder can significantly impair relationships, work, and overall quality of life.
- Psychotherapy:
- Cognitive Behavioral Therapy (CBT):
- Helps challenge and reframe delusional beliefs.
- Focuses on reducing distress and improving coping mechanisms.
- Supportive Therapy:
- Builds trust and helps individuals manage the impact of their beliefs on daily life.
- Family Therapy:
- Educates family members on how to support the individual effectively.
- Cognitive Behavioral Therapy (CBT):
- Medication:
- Antipsychotics:
- Commonly accepted treatment that is so-called – first-line.
- Drugs like Risperidone, Olanzapine, or Aripiprazole can reduce the intensity of delusions.
- Adjunctive Therapy:
- Antidepressants or anxiolytics may be used if mood symptoms or anxiety are present.
- Antipsychotics:
- Social Interventions:
- Encouraging social engagement and addressing isolation.
- Providing vocational and occupational support.
Prognosis
- The course varies depending on:
- The subtype of delusion.
- The level of insight.
- Early detection and treatment.
- With proper treatment, many individuals can lead relatively normal lives.
F22 delusional disorder vs. other conditions
- Schizophrenia:
- Delusional disorder lacks prominent hallucinations, disorganized speech, and negative symptoms like apathy.
- Bipolar Disorder:
- Delusions in bipolar disorder occur during mood episodes (mania or depression), unlike the persistent delusions in F22.
- Obsessive-Compulsive Disorder (OCD):
- Obsessions in OCD are intrusive and recognized as irrational, unlike delusions, which are firmly held beliefs.
Sources:
- American Psychiatric Association, 2022. Diagnostic and Statistical Manual of Mental Disorders (5th ed., text rev.). American Psychiatric Publishing.
- Arciniegas, D.B., 2021. Psychosis. Continuum (Minneap Minn), 27(4), pp. 1010-1036. doi:10.1212/CON.0000000000001010
- Freudenmann, R.W. & Lepping, P., 2009. Delusional infestation. Clinical Microbiology Reviews, 22(4), pp. 690-732. doi:10.1128/CMR.00013-09
- Grover, S., Biswas, P. & Avasthi, A., 2014. Delusional disorder: Etiology, diagnosis, and management. Current Opinion in Psychiatry, 27(3), pp. 214-219. doi:10.1097/YCO.0000000000000060
- Manschreck, T.C. & Khan, N.L., 2006. Recent advances in the treatment of delusional disorder. Canadian Journal of Psychiatry, 51(2), pp. 114-119. doi:10.1177/070674370605100208
- National Institute for Health and Care Excellence (NICE), 2023. Psychosis and schizophrenia in adults: prevention and management. [online] Available at: https://www.nice.org.uk/guidance/cg178 [Accessed 10 June 2025].
- World Health Organization (WHO), 2023. ICD-10 Version:2019. [online] Available at: https://icd.who.int/browse10/2019/en#/F22 [Accessed 10 June 2025].
- Yamada, K. & Sato, T., 2021. Delusional disorder: Epidemiology, clinical characteristics, and management. Journal of Clinical Psychiatry, 82(2), pp. 20r13368. doi:10.4088/JCP.20r13368