The F23 category in the ICD-10 refers to Acute and Transient Psychotic Disorders (ATPD). These disorders are serious mental health conditions marked by a sudden appearance of psychotic symptoms, including delusions, hallucinations, and changes in perception. These disorders develop rapidly and typically resolve within a few weeks to months. Below is a comprehensive overview tailored for medical professionals:
- Onset: Sudden and acute, with psychotic symptoms developing over two weeks or less.
- Duration: Usually transient, resolving within 3 months. However, some cases may transition to chronic psychotic disorders.
- Course: Often fluctuating, with the possibility of complete remission or progression to more chronic conditions like schizophrenia.
Types of F23 disorders
Acute and transient psychotic disorders in ICD-10 represent a distinct neuropsychiatric phenomenon where individuals experience profound perceptual disruptions lasting between several days and one month, with complete or near-complete symptom resolution. Unlike chronic psychotic conditions, these episodes emerge rapidly, often in response to significant psychological stressors, and demonstrate remarkable neurological plasticity.
For a F23 diagnosis, medical specialists must observe:
- Acute onset (typically within two weeks)
- Polymorphic psychotic symptoms
- Substantial emotional turbulence
- Preserved fundamental personality structure
- Minimal long-term functional impairment
- Complete or near-complete symptomatic recovery
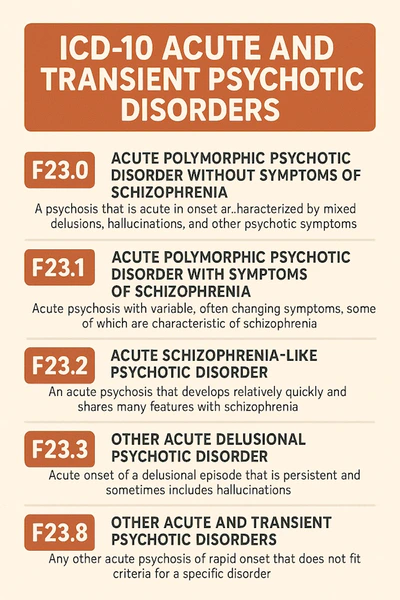
The ICD-10 distinguishes between several subtypes of F23 diagnosis based on symptoms and underlying causes:
F23.0: Acute polymorphic psychotic disorder without symptoms of schizophrenia
Characterized by highly variable symptom manifestations without rigid schizophrenic structural patterns. Patients experience rapid mood shifts, perceptual distortions, and emotional lability. Hallucinations might be fragmented, delusions unstable, and emotional responses dramatically fluctuating. The key distinguishing feature is the transient, non-systematized nature of psychotic experiences.
Characteristics:
- Rapidly changing psychotic symptoms.
- Hallucinations and delusions may be present but are fleeting and not well-structured.
- Emotional instability (mood swings) is prominent.
Differentiation:
- Symptoms are less structured than in schizophrenia.
- Lack of persistent core symptoms like formal thought disorder.
Diagnostic nuances:
- Symptoms emerge quickly
- Emotional responses remain relatively intact
- High variability in perceptual experiences
- Potential complete symptomatic resolution
- Minimal cognitive deterioration
F23.1: Acute polymorphic psychotic disorder with symptoms of schizophrenia
This subtype introduces more structured psychotic elements reminiscent of schizophrenic experiences. Patients demonstrate more organized hallucinatory content, potentially developing brief but more coherent delusional frameworks. The fundamental difference from chronic schizophrenia lies in the episode’s transient nature and potential for complete recovery.
Characteristics:
- Acute onset of rapidly shifting psychotic symptoms, similar to F23.0.
- Includes symptoms characteristic of schizophrenia (e.g., thought insertion, delusions of control, auditory
- hallucinations).
- Emotional instability may still be present.
Differentiation:
- Symptoms meet some but not all criteria for schizophrenia.
- Shorter duration compared to chronic schizophrenia.
Key Diagnostic Markers:
- Presence of schizophrenia-like symptom clusters
- Preserved underlying personality structure
- Potential brief catatonic manifestations
- Rapid symptom emergence and resolution
- Higher potential for recurrence compared to non-schizophrenic variants
F23.2: Acute schizophrenia-like psychotic disorder
This diagnostic space accommodates psychotic experiences that do not precisely fit preceding categories but maintain core F23 diagnostic principles. Medical specialists utilize this classification when encountering unique psychotic presentations that challenge traditional diagnostic boundaries.
Characteristics:
- Prominent schizophrenia symptoms, such as:
- Delusions.
- Hallucinations (especially auditory).
- Patient has disorganized thoughts and speech.
- Less emotional instability compared to F23.0 or F23.1.
Differentiation:
- Onset is acute, unlike schizophrenia’s insidious onset.
- Duration is shorter than 6 months (beyond which it may be reclassified as schizophrenia).
F23.3: Other acute predominantly delusional psychotic disorders
Characteristics:
- Dominance of well-structured delusions (e.g., paranoid delusions).
- Few or no hallucinations.
- Minimal emotional instability.
Differentiation:
- Distinguished from delusional disorders (F22) by its acute onset and shorter duration.
F23.8: Other acute and transient psychotic disorders
Characteristics:
- Includes presentations not covered by the above subtypes.
- Symptoms can be a mix of psychotic features without clear categorization.
Differentiation:
- Catch-all category for atypical presentations.
F23.9: Acute and transient psychotic disorder, unspecified
Characteristics:
- Used when there is insufficient information to classify the disorder into a specific subtype.
Differentiation:
- Lack of diagnostic detail limits further classification.
Symptoms
Common symptoms across all F23 disorders include:
Delusions:
- Paranoid, grandiose, or various bizarre beliefs.
- Frequently unstable or poorly systematized.
Hallucinations:
- Auditory hallucinations are most common.
- Possible visual and/or tactile hallucinations can be present in patient.
Disorganized Thinking:
- Thought blocking, incoherence, or derailment.
Emotional Disturbance:
- Severe mood swings (e.g., euphoria, irritability, anxiety).
- Emotional unpredictability is more pronounced in F23.0 and F23.1.
Behavioral Changes:
- Agitation or catatonia.
- Unpredictable, socially inappropriate actions.
Differential diagnosis
Key disorders to differentiate from F23 include:
1. Schizophrenia (F20)
In schizophrenia:
- Duration: Symptoms persist for more than 6 months.
- Onset: Insidious rather than acute.
- Symptoms: More persistent core symptoms (e.g., thought disorder, negative symptoms).
2. Delusional disorders (F22)
In F22 delusional disorder:
- Duration: Chronic, often lasting years.
- Symptoms: Predominantly delusions without significant emotional instability or hallucinations.
3. Mood disorders with psychotic features (F30–F39)
- Symptoms: Psychotic symptoms are secondary to mood episodes (mania or depression).
- Mood: Persistent and central to the clinical presentation.
4. Substance-induced psychotic disorder
- History: Recent substance use or withdrawal.
- Course: Symptoms resolve with abstinence.
5. Organic causes (e.g., delirium, encephalitis, epilepsy)
- Features: Presence of neurological signs, cognitive deficits, or abnormal imaging/laboratory results.
- Course: Resolves with treatment of the underlying condition.
6. Borderline personality disorder (F60.3)
- Symptoms: Emotional instability and transient psychotic episodes.
- Course: Chronic with episodic flare-ups rather than an acute onset.
To diagnose F23 disorders, the medical specialist must observe the following:
Timeframe:
- Acute onset (symptoms develop within 2 weeks).
- Duration typically less than 3 months.
Symptomatology:
- Psychotic features such as delusions and/or hallucinations may be present.
- Emotional instability or disorganized behavior (varies by subtype).
Exclusion:
- Rule out organic causes (e.g., head trauma, infection).
- Exclude substance use or withdrawal as the primary cause.
Long-term outlook
Most patients with F23 disorders demonstrate:
- High recovery potential
- Minimal chronic psychological impairment
- Capacity for complete symptomatic resolution
Pharmacological:
- Antipsychotics: For severe symptoms (e.g., Risperidone, Olanzapine).
- Mood stabilizers: In cases with significant emotional instability.
Psychosocial Support:
- Crisis intervention and family education.
- Address stressors triggering the episode.
Follow-Up:
- Regular monitoring to ensure symptom resolution.
- Reassess if symptoms persist beyond 3 months to exclude schizophrenia.
Prognosis
- High likelihood of full recovery with timely treatment.
- Risk of progression to chronic psychotic disorders (e.g., schizophrenia) in a subset of patients.