Induced Delusional Disorder, coded as F24 in the ICD-10, is a rare psychiatric condition where a delusion is shared between two or more individuals who are in close relationship, often referred to as folie à deux.
Induced delusional disorder represents a fascinating phenomenon where psychotic symptoms, primarily delusions, are transmitted from a person with an established psychotic disorder (the primary patient) to one or more other individuals (the secondary patients) who are typically in a close emotional relationship and often living in relative social isolation.
This condition typically involves a dominant individual with an established delusional belief who influences another, usually more passive or dependent person, to adopt the same delusion. The disorder is more common in isolated settings, such as families or small groups with limited social interactions.
Symptoms and clinical presentation
The secondary patient adopts the delusional system of the primary patient and shows genuine conviction in these transferred beliefs. The content of shared delusions commonly involves persecution, grandiosity, or somatic concerns. Secondary patients frequently demonstrate less severe symptoms compared to the primary case, and their delusional beliefs might be more circumscribed or less elaborated.
The symptoms of F24 include:
1. Shared Delusional Beliefs: The central feature is the presence of a delusion that originates in one person and is adopted by another. These beliefs often involve persecution, grandeur, or other themes commonly seen in primary psychotic disorders.
2. Submissive Personality in the Secondary Individual: The influenced person often has a close, dependent relationship with the inducer and may share psychological vulnerabilities such as low self-esteem or social isolation.
3. Strong Emotional Connection: The individuals involved often have an intensely close emotional bond, which facilitates the transmission of delusions.
4. Improvement with Separation: The secondary individual may show significant improvement or even a complete resolution of symptoms when separated from the primary delusional person.
5. Absence of Psychotic Illness in the Secondary Individual: The influenced person usually lacks a history of independent psychotic disorders. The shared delusion is context-dependent and linked to the relationship.
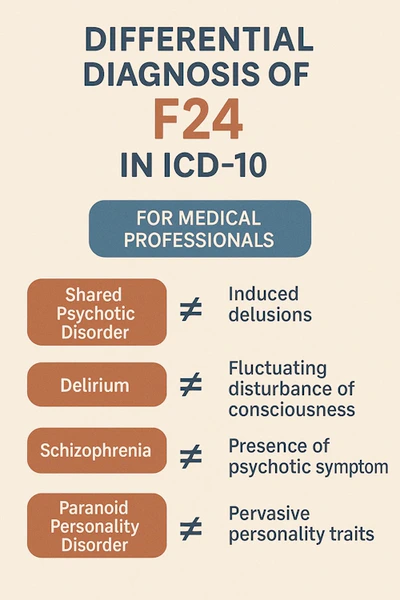
Differential diagnosis
To accurately diagnose F24, it is crucial to differentiate it from other psychiatric disorders.
1. Schizophrenia (F20):
Schizophrenia involves primary psychotic symptoms such as hallucinations, thought disorder, and negative symptoms. In contrast, F24 is limited to delusional beliefs and is contextually dependent on the relationship.
2. Delusional disorder (F22):
Unlike F24, delusional disorder is characterized by persistent delusions that arise independently and are not shared between individuals.
4. Mood disorders with psychotic features (F31.2, F32.3):
In mood disorders, delusions are usually mood-congruent and secondary to affective disturbances, which is not the case in F24.
5. Dependent personality disorder (F60.7):
Dependency may be present in F24 but does not explain the presence of delusional beliefs, which are the defining feature of this disorder.
6. Cultural or religious beliefs:
Shared beliefs in cultural or religious contexts should not be mistaken for F24 unless they are delusional, idiosyncratic, and impair functioning.
7. Substance-induced psychosis (F1x.5):
It is important to rule out drug-induced psychosis, which can mimic delusional states but is linked to substance use and not interpersonal dynamics.
8. Psychosis due to another medical condition:
Neurological conditions or other physiological causes of psychosis need to be excluded by thorough medical evaluation.
Diagnostic considerations
Critical considerations for clinicians:
When evaluating potential cases, psychiatrists should pay particular attention to:
- The exact chronology of symptom development in both individuals
- The nature and quality of the relationship between involved parties
- The degree of social isolation and environmental factors
- The presence of pre-existing psychiatric conditions or personality traits
- The extent of shared vs. independent elements in the delusional system
Documentation should carefully detail these aspects to support accurate diagnosis and treatment planning.
The diagnosis of F24 relies on clinical assessment and history-taking. Key considerations include:
- Relationship Dynamics: Evaluating the power dynamics, dependency, and emotional closeness between individuals is crucial.
- Independent Psychopathology: Assess whether the secondary individual has delusions outside the influence of the primary person.
- Response to Separation: Temporary or permanent separation often provides diagnostic clarity, as the secondary individual’s symptoms typically resolve when isolated from the inducer.
- Cultural Context: Determine whether the shared beliefs are delusional within the cultural framework or reflect a shared worldview.
Management
Treatment focuses on:
- Interview both individuals: If possible, interview both the primary and secondary cases together and separately. Look for the initiation of delusions in one person and their subsequent adoption by another.
- History taking: Detailed history should focus on the onset of delusions, the nature of the relationship, and any history of mental health issues in both individuals.
- Separation: Physical and emotional separation of the individuals is often necessary.
- Psychotherapy: Individual therapy for both parties can address underlying vulnerabilities and maladaptive dynamics.
- Medication: The primary individual may require antipsychotics for their delusions, while the secondary individual usually does not unless independent psychiatric symptoms develop.
- Family therapy: In cases involving families, therapy can address relational patterns and prevent recurrence.
When diagnosing F24, it is vital for clinicians to identify the unique interpersonal dynamics underlying this condition. Proper diagnosis and management depend on careful differentiation from other psychotic and personality disorders, as well as attention to the psychosocial context.
Sources:
- Bourgeois, J.A., Sabes, J.H., Servis, M.E. & O’Halloran, J.P., 2021. Folie a Deux: Shared Psychotic Disorder in a Medical Unit. Case Reports in Psychiatry, 2021, Article ID 8487833. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC8487833/
- Mastromo, D. & De Panfilis, A., 2021. Shared psychotic disorder: A case report. Early Clinical Interventions in Psychiatry, 1(1), pp.1-5. Available at: https://www.pagepressjournals.org/ecj/article/download/11599/11309/69823
- Cipriani, G., Vedovello, M., Ulivi, M., Nuti, A. & Lucetti, C., 2018. A Contagious Disorder: Folie à Deux and Dementia. American Journal of Alzheimer’s Disease & Other Dementias, 33(8), pp.547-551. doi:10.1177/1533317518772060
- Cambridge University Press, 2023. Folie a deux / induced delusional disorder – case report and literature review. European Psychiatry, 66(S1), pp.S1038-S1039. Available at: https://www.cambridge.org/core/journals/european-psychiatry/article/folie-a-deux-induced-delusional-disorder-case-report-and-literature-review/DDB1103AC6690C76DAB790AC4F9DAF3A
- Ranjan, R. & Kumar, S., 2023. Folie a deux / induced delusional disorder – case report and literature review. European Psychiatry, 66(S1), pp.S1038-S1039. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC10479191/
- Bourgeois, J.A., Servis, M.E. & O’Halloran, J.P., 2021. Article ID 8811140. Available at: https://onlinelibrary.wiley.com/doi/10.1155/2022/8811140
- Ghaffari Nejad, A., 2020. Uncommon Presentation: Folie à deux (Case Study). SSRN Electronic Journal. Available at: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3747587