A heart attack happens when blood flow to part of the heart muscle is severely reduced or blocked. Without quick treatment, that section of heart muscle can become permanently damaged. Every minute counts during a heart attack. Knowing the warning signs and taking immediate action can save a life—possibly your own or someone you love.
This guide will help you recognize heart attack symptoms, understand when to seek emergency help, and know what actions to take while waiting for medical assistance. It’s written specifically for people with no medical background, including older adults living alone and family members who may need to recognize these warning signs in their loved ones.
Common warning signs of a heart attack
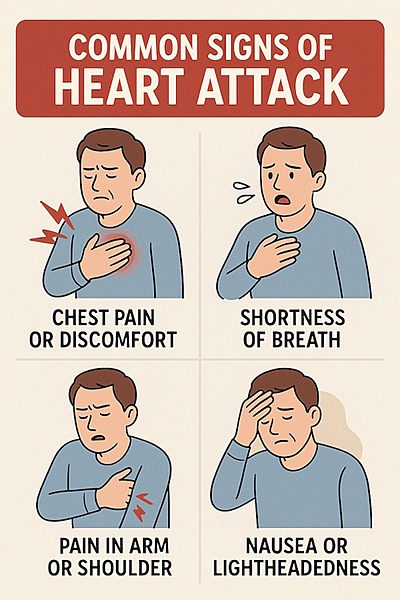
Heart attacks often don’t appear the way they’re portrayed in films. The symptoms can be dramatic or subtle, and they may vary between men and women. Here are the most common warning signs:
Chest discomfort
What it feels like:
- A sensation of pressure, tightness, heaviness, or discomfort in the middle of the chest
- Can last for more than a few minutes, or might go away and come back
- Might feel like uncomfortable pressure, squeezing, fullness, or pain
- Some describe it as “an elephant sitting on my chest” or “a tight band around my chest”
Important to know: Not all heart attacks cause severe chest pain. For some people, especially women, older adults, and people with diabetes, the sensation might be mild discomfort that’s easy to dismiss.
Discomfort in other areas of the upper body
Pain or discomfort might spread beyond your chest to:
- One or both arms (especially the left arm)
- Back
- Neck
- Jaw
- Stomach/upper abdomen
- Between the shoulder blades
Shortness of breath
- May occur with or without chest discomfort
- Feeling like you can’t catch your breath
- Needing to sit down to try to breathe more easily
- Breathing that feels more difficult than normal
Other Common Signs
- Cold sweat (sudden sweating with cool, clammy skin)
- Nausea or vomiting
- Lightheadedness or sudden dizziness
- Unusual fatigue or weakness (extreme tiredness that is new or unexpected)
- Sense of doom (feeling like something terrible is about to happen)
- Rapid or irregular heartbeat
- Indigestion or heartburn-like discomfort
Less common signs
These symptoms are less common but still important to recognize:
- Unexplained anxiety or nervousness
- Confusion or trouble thinking clearly (especially in older adults)
- Sleep disturbances
- Fainting or near-fainting
Special considerations for different groups
Women’s heart attack symptoms
Women are more likely than men to experience:
- Shortness of breath
- Nausea/vomiting
- Back or jaw pain
- Fatigue and weakness
- Heartburn-like symptoms
- Dizziness
Women often don’t experience the classic “crushing chest pain” that men typically report. This is one reason heart attacks in women are more frequently missed or misdiagnosed.
Older adults
Older adults may experience:
- Confusion or disorientation
- Extreme fatigue
- Shortness of breath with minimal exertion
- Dizziness or falls
- Reduced stamina without chest pain
People with diabetes
People with diabetes may have:
- Milder symptoms or no chest pain (due to nerve damage from diabetes)
- Unusual fatigue
- Shortness of breath
- Dizziness
- Nausea
“Silent” heart attacks
About 20% of heart attacks are “silent,” meaning they happen without the person knowing it. These are more common in:
- Older adults
- People with diabetes
- Women
Signs you may have had a silent heart attack include:
- Unexplained fatigue that persists for days
- Discomfort in chest, arms, or jaw that comes and goes
- Shortness of breath that worsens with activity
- Sleep disturbances
- Heartburn or indigestion that doesn’t respond to antacids
When to take action: the importance of time
DO NOT WAIT to see if symptoms go away on their own. Heart attacks cause progressive damage to heart muscle—the longer treatment is delayed, the more damage occurs.
Take immediate action if:
- Symptoms last longer than 5 minutes
- Symptoms are severe or getting worse
- You have any chest discomfort along with other symptoms like shortness of breath, nausea, or lightheadedness
Remember: It’s always better to call for help and find out it’s not a heart attack than to wait and suffer permanent heart damage or worse.
Steps to take during a suspected heart attack
If you think you’re having a heart attack:
- Call emergency services immediately (911 in US, 112 or 999 in many other countries)
- Don’t drive yourself to the hospital
- Don’t have someone else drive you unless there’s absolutely no other option
- Emergency responders can begin treatment as soon as they arrive
- Chew and swallow an aspirin (if you’re not allergic to aspirin)
- Use a regular, non-coated aspirin
- Chewing gets the medication into your bloodstream faster than swallowing it whole
- Standard adult dose is 325 mg (or four low-dose 81 mg tablets)
- Skip this step if you have a known aspirin allergy
- Sit or lie down in a comfortable position
- Try to remain calm
- Loosen tight clothing
- If sitting, keep legs uncrossed
- If lying down, elevate your head and shoulders slightly
- Prepare for emergency responders
- Unlock your door if possible
- If you’re alone, try to get to a phone and stay on the line with emergency services
- Have a list of your medications ready if possible
If you witness someone having a suspected heart attack:
- Call emergency services (911)
- Put the call on speaker phone so you can continue to help the person
- Help them into a comfortable position
- Semi-sitting position with knees bent is often best
- Support their back and head
- Loosen tight clothing like belts, ties, collars
- Give aspirin if available and no known allergies
- Ask if they’re allergic before giving aspirin
- Have them chew one adult aspirin (325 mg) or four low-dose aspirin (81 mg each)
- Monitor breathing and consciousness
- Stay with them until help arrives
- Be prepared to perform CPR if they become unresponsive and stop breathing normally
- If trained and an AED (Automated External Defibrillator) is available, use it according to its instructions
- Be ready to provide information to paramedics
- When symptoms started
- What the person was doing when symptoms began
- Their medical history if you know it
- Any medications they take
If the person becomes unresponsive
If someone having a heart attack loses consciousness and is not breathing normally:
- Begin CPR immediately
- Push hard and fast in the center of the chest (at least 2 inches deep at a rate of 100-120 compressions per minute)
- Allow the chest to fully recoil between compressions
- Minimize interruptions in compressions
- If untrained in CPR, perform “Hands-Only CPR” – push hard and fast in the center of the chest to the beat of “Stayin’ Alive” by the Bee Gees
- Use an AED if available
- Follow the voice prompts
- Apply pads to bare chest as shown in the diagrams
- Allow the device to analyze and deliver a shock if advised
- Continue CPR until help arrives
- Switch compressors every 2 minutes if another person is available to help
- Do not stop except when the AED is analyzing or delivering a shock
Heart attack vs. cardiac arrest
It’s important to understand the difference:
Heart Attack: The heart continues to beat but blood flow to part of the heart is blocked. The person is usually conscious and breathing.
Cardiac Arrest: The heart suddenly stops beating altogether. The person is unconscious, not breathing normally, and needs immediate CPR.
A heart attack and cardiac arrest are distinct conditions, though a heart attack can sometimes trigger cardiac arrest.
Both require immediate emergency action.
Prevention and preparation
Know your risk factors
Common risk factors for heart attack include:
- High blood pressure
- High cholesterol
- Smoking
- Diabetes
- Family history of heart disease
- Age (men over 45, women over 55)
- Obesity
- Physical inactivity
- Unhealthy diet
- Stress
- Excessive alcohol consumption
Create an emergency plan
- Keep emergency numbers visible
- Post emergency numbers by your phones
- Program them into your mobile phone
- If you live by yourself, think about using a medical alert device
- Prepare an information sheet
- List all medications and doses
- Note medical conditions
- Include allergies
- Add emergency contacts
- Keep this information in your wallet or on your refrigerator (where emergency responders often look)
- Learn CPR and basic first aid
- Take a class or learn “Hands-Only CPR”
- Encourage family members to learn as well
- Know the location of nearby AEDs
- Check your workplace, gym, shopping centers, and other public places you frequent
Talk to your doctor about:
- Your personal risk factors for heart attack
- Warning signs that might be specific to your health condition
- Whether you should carry aspirin
- Any unusual symptoms you’ve experienced
Common concerns and questions
“How can I tell if it’s just indigestion?”
Heart attack symptoms can be confused with indigestion, but consider these differences:
- Heart-related chest pain typically isn’t affected by your body position or by burping
- Heart pain often spreads to other areas like the arm, jaw, or back
- Heart symptoms frequently include other signs like shortness of breath or sweating
When in doubt, seek emergency help.
“I don’t want to bother emergency services if it’s nothing serious.”
Emergency responders would rather come to you and find it’s not a heart attack than have you delay calling and suffer serious damage. Don’t let embarrassment or concern about “false alarms” prevent you from seeking help.
“I had similar symptoms before and it wasn’t a heart attack.”
Heart attack symptoms can vary from one event to another. Previous symptoms that weren’t a heart attack don’t guarantee current symptoms are also not serious. Always take chest discomfort and related symptoms seriously.
“What if I can’t access emergency services?”
If you absolutely cannot call emergency services or get to a hospital:
- Take an aspirin if available and you’re not allergic
- Ask someone to take you to the closest emergency room
- Don’t drive yourself unless there is absolutely no alternative
Conclusion
Remember these key points:
- Know the warning signs
- Take action quickly if symptoms occur
- Call emergency services immediately
- Follow emergency dispatcher instructions
- Be prepared with an emergency plan
This guide is meant to provide information about recognizing and responding to heart attack symptoms, but it’s not a substitute for professional medical advice. Always consult with your healthcare provider about your specific health concerns and risks.
Additional Resources
- American Heart Association: www.heart.org
- British Heart Foundation: www.bhf.org.uk
- Heart and Stroke Foundation of Canada: www.heartandstroke.ca
- Heart Foundation (Australia): www.heartfoundation.org.au
